Fill Out a Valid Progress Notes Template
Guide to Writing Progress Notes
After obtaining the Progress Notes form, it’s important to fill it out accurately to ensure that all necessary information is documented. Follow these steps to complete the form correctly.
- Date: Write the current date at the top of the form.
- Patient's Identification: Fill in the patient's name in the format of last name, first name, and middle initial. Include the patient's grade, rank, or rate, as applicable, and the name of the hospital or medical facility.
- Register Number: Enter the patient’s register number in the designated space.
- Ward Number: Specify the ward number where the patient is located.
- Progress Notes: Document the relevant progress notes in the space provided. Ensure that all entries are clear and concise.
Once you have completed the form, review it for any errors before submitting it to the appropriate department. This will help maintain accurate medical records.
Document Breakdown
| Fact Name | Details |
|---|---|
| Form Purpose | The Progress Notes form is used to document a patient's medical history and treatment updates. |
| Identification Requirements | It requires patient identification details, including name, grade, rank, rate, and the medical facility. |
| Standardization | This form is a standardized document, specifically Standard Form 509, revised in July 1991. |
| Governing Laws | In the United States, the form is prescribed under regulations from GSA/ICMR and FIRMR (41 CFR 201-9.202-1). |
| Usage Context | Progress Notes are typically used in hospitals and medical facilities for consistent record-keeping. |
| Continuity of Care | These notes are essential for ensuring continuity of care by providing updates on patient status. |
FAQ
What is the purpose of the Progress Notes form?
The Progress Notes form serves to document the ongoing care and treatment of a patient. It provides a structured way to record observations, treatment plans, and any changes in the patient's condition. This documentation is essential for maintaining accurate medical records and ensuring continuity of care among healthcare providers.
What information is required on the Progress Notes form?
The form requires specific patient identification details, including:
- Patient's name (last, first, middle)
- Grade, rank, or rate, as applicable
- Hospital or medical facility name
- Register number
- Ward number
These details help to accurately identify the patient and link the notes to their medical records.
How should the Progress Notes be completed?
Progress Notes can be completed using either typed or handwritten entries. It is important to ensure that all information is clear and legible. The date of the entry must be included, and any observations or notes should be concise yet detailed enough to convey the necessary information about the patient's status and care.
Who is responsible for filling out the Progress Notes?
Healthcare providers who are involved in the patient's care, such as doctors, nurses, or therapists, are responsible for filling out the Progress Notes. Each provider should document their observations and interventions to create a comprehensive record of the patient's treatment.
Can additional pages be used for Progress Notes?
Yes, if more space is needed, providers can continue their notes on the reverse side of the form. It is important to maintain clarity and organization when adding additional information to ensure that all notes are easily understandable.
What is the significance of using Standard Form 509?
Standard Form 509 is prescribed by the General Services Administration (GSA) and is designed to ensure uniformity in medical record-keeping. Using this standardized form helps to maintain consistency across different healthcare facilities and providers, which is crucial for effective communication and quality patient care.
Fill out Other Forms
Gift Voucher Template - Encourage creativity in gift selection.
Florida State Return - Authorized representatives can represent taxpayers during IRS or state tax proceedings.
To assist you in preparing for the future, the Last Will and Testament preparation guide is here to simplify the process of crafting important end-of-life plans. This document is vital for ensuring your wishes are honored and legally binding, safeguarding your loved ones during difficult times. For further insights, visit the Last Will and Testament form resource.
Hvac Job Application - Strong record of safety compliance and practices.
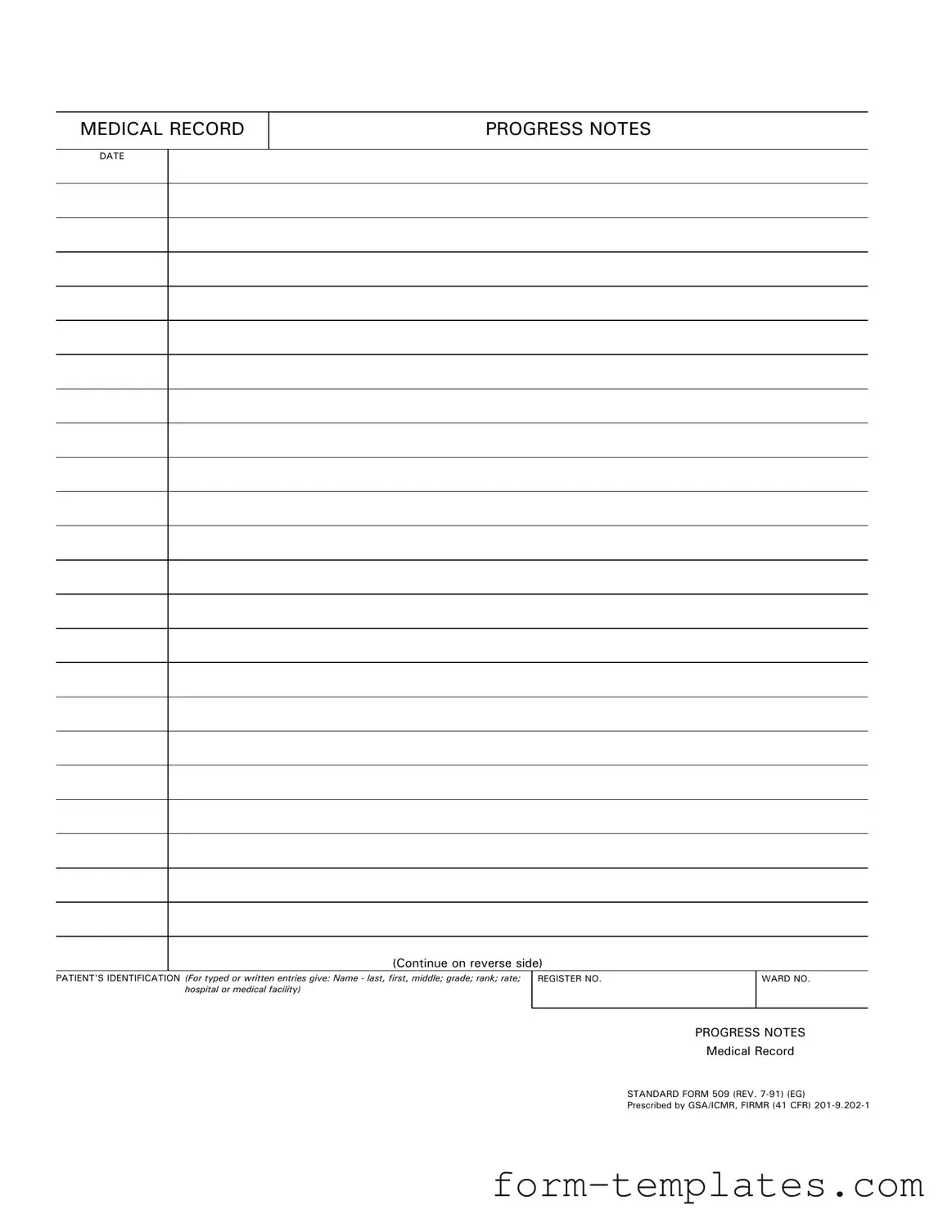
Progress Notes Example
MEDICAL RECORD
PROGRESS NOTES
DATE
(Continue on reverse side)
PATIENT'S IDENTIFICATION (For typed or written entries give: Name - last, first, middle; grade; rank; rate; hospital or medical facility)
REGISTER NO. |
WARD NO. |
|
|
PROGRESS NOTES
Medical Record
STANDARD FORM 509 (REV.
Prescribed by GSA/ICMR, FIRMR (41 CFR)
PROGRESS NOTES
DATE
STANDARD FORM 509 (REV.