Fill Out a Valid Advance Beneficiary Notice of Non-coverage Template
Guide to Writing Advance Beneficiary Notice of Non-coverage
Completing the Advance Beneficiary Notice of Non-coverage (ABN) form is an important step in understanding your healthcare coverage options. Once you have the form filled out, you can discuss your choices with your healthcare provider. Follow these steps to ensure the form is completed accurately.
- Obtain the ABN form from your healthcare provider or download it from a reliable source.
- Begin by entering your personal information at the top of the form. This includes your name, address, and Medicare number.
- Identify the service or item that may not be covered by Medicare. Clearly describe the service in the designated section.
- In the next section, indicate the reason why you believe the service may not be covered. Be specific about your understanding of coverage limitations.
- Review the options provided on the form. You will need to select whether you want to receive the service or not, understanding the potential costs involved.
- Sign and date the form at the bottom. This confirms that you have received the notice and understand your options.
- Make a copy of the completed form for your records before submitting it to your healthcare provider.
After completing the ABN form, discuss it with your healthcare provider to clarify any questions about the services and potential costs. This will help you make informed decisions regarding your healthcare options.
Document Breakdown
| Fact Name | Description |
|---|---|
| Purpose | The Advance Beneficiary Notice of Non-coverage (ABN) informs beneficiaries that Medicare may not cover a service or item. |
| Required Use | Providers must issue an ABN when they believe Medicare will deny payment for a service or item. |
| Beneficiary Rights | Beneficiaries have the right to refuse services after receiving an ABN. |
| Signature Requirement | Beneficiaries must sign the ABN to acknowledge their understanding of potential non-coverage. |
| State Variations | Some states may have specific laws governing the use of ABNs. For example, California has additional regulations under the California Code of Regulations. |
| Delivery Method | The ABN can be delivered in person, by mail, or electronically, depending on the provider's policies. |
| Effective Date | The ABN must be issued before the service is provided to ensure beneficiaries are informed in advance. |
| Documentation | Providers must keep a copy of the signed ABN in the beneficiary's medical record for compliance purposes. |
| Impact on Billing | If a beneficiary signs the ABN and the service is not covered, they are responsible for payment. |
| Form Updates | The ABN form is subject to updates by the Centers for Medicare & Medicaid Services (CMS), and providers must use the most current version. |
FAQ
What is the Advance Beneficiary Notice of Non-coverage (ABN)?
The Advance Beneficiary Notice of Non-coverage, commonly referred to as the ABN, is a form that healthcare providers give to Medicare beneficiaries. This form informs patients that a service or item may not be covered by Medicare. It allows patients to make informed decisions about their care and financial responsibilities.
When should I receive an ABN?
You should receive an ABN when your healthcare provider believes that Medicare may not pay for a specific service or item. This typically occurs before the service is provided. The provider is required to give you the ABN to ensure you understand the potential costs involved.
What happens if I don’t sign the ABN?
If you choose not to sign the ABN, you may still receive the service, but you might be responsible for the full cost if Medicare denies coverage. Signing the ABN indicates that you understand the potential for non-coverage and accept financial responsibility if that occurs.
What should I do if I receive an ABN?
When you receive an ABN, take the time to read it carefully. Consider the following steps:
- Review the service or item listed on the ABN.
- Understand why your provider believes it may not be covered.
- Decide whether you want to proceed with the service, knowing you may have to pay out of pocket.
- Ask your provider any questions you may have about the form or the service.
Can I appeal if Medicare denies coverage after I sign an ABN?
Yes, you can appeal a Medicare denial even after signing an ABN. If you believe the service should be covered, you have the right to file an appeal. This process involves submitting a request for reconsideration to Medicare, explaining why you think the service should be covered.
Will I be charged if I receive an ABN?
Is the ABN the same for all services?
No, the ABN can vary based on the service or item being provided. Different services may have different reasons for potential non-coverage. Your healthcare provider will fill out the ABN with specific details related to the service you are receiving.
How does the ABN affect my Medicare benefits?
Where can I find more information about the ABN?
For more information about the ABN, you can visit the official Medicare website or contact Medicare directly. Additionally, your healthcare provider can answer questions and provide guidance on how the ABN may affect your specific situation.
Fill out Other Forms
90 Day Notice to Vacate California - This 90-Day Notice can trigger thoughts about finding new housing for tenants.
To ensure a smooth and efficient background verification process, it is essential to utilize the correct documents. One such important tool is the Fillable Blank Check, which must be completed as part of the CID Name Check Request procedure. By properly filling out all required forms, you can help streamline the identification process and ensure that accurate information is retrieved.
Where to Find Old Immunization Records - A designated area for the doctor’s office or clinic ensures accurate record-keeping.
Advance Beneficiary Notice of Non-coverage Example
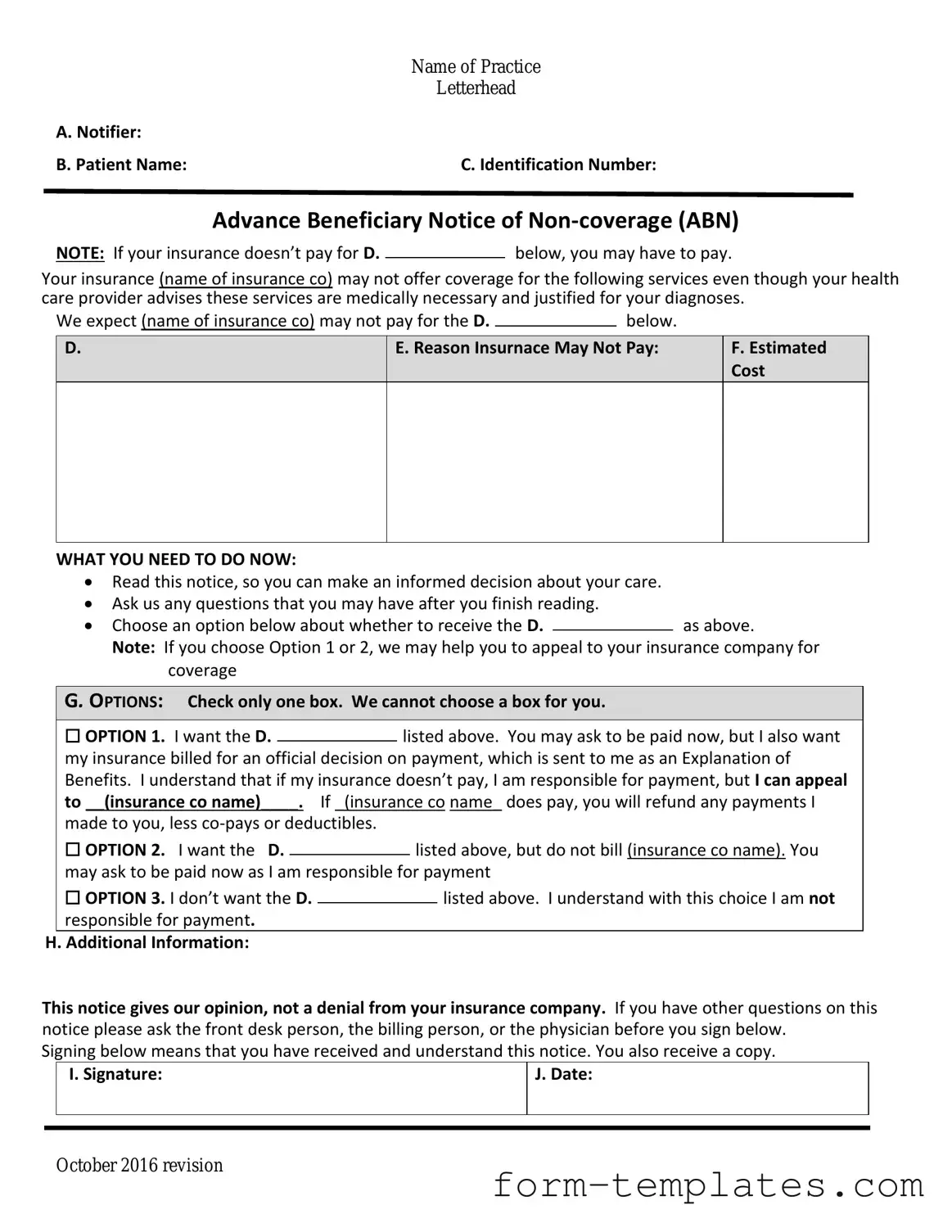
|
Name of Practice |
|
Letterhead |
A. Notifier: |
|
B. Patient Name: |
C. Identification Number: |
Advance Beneficiary Notice of
NOTE: If your insurance doesn’t pay for D.below, you may have to pay.
Your insurance (name of insurance co) may not offer coverage for the following services even though your health care provider advises these services are medically necessary and justified for your diagnoses.
We expect (name of insurance co) may not pay for the D. |
|
below. |
|
D.
E. Reason Insurnace May Not Pay:
F.Estimated Cost
WHAT YOU NEED TO DO NOW:
Read this notice, so you can make an informed decision about your care.
Ask us any questions that you may have after you finish reading.
Choose an option below about whether to receive the D.as above.
Note: If you choose Option 1 or 2, we may help you to appeal to your insurance company for coverage
G. OPTIONS: Check only one box. We cannot choose a box for you.
|
☐ OPTION 1. I want the D. |
|
listed above. You may ask to be paid now, but I also want |
||||
|
|
||||||
|
my insurance billed for an official decision on payment, which is sent to me as an Explanation of |
||||||
|
Benefits. I understand that if my insurance doesn’t pay, I am responsible for payment, but I can appeal |
||||||
|
to __(insurance co name)____. If _(insurance co name_ does pay, you will refund any payments I |
||||||
|
made to you, less |
|
|
|
|||
|
☐ OPTION 2. I want the D. |
|
|
listed above, but do not bill (insurance co name). You |
|||
|
|
|
|||||
|
may ask to be paid now as I am responsible for payment |
||||||
|
☐ OPTION 3. I don’t want the D. |
|
|
|
listed above. I understand with this choice I am not |
||
|
|
|
|
||||
|
responsible for payment. |
|
|
|
|||
H. Additional Information: |
|
|
|
||||
This notice gives our opinion, not a denial from your insurance company. If you have other questions on this notice please ask the front desk person, the billing person, or the physician before you sign below.
Signing below means that you have received and understand this notice. You also receive a copy.
|
I. Signature: |
J. Date: |
|
|
|
|
|
|
October 2016 revision